Prenatal Care: The Pros and Cons of the Obstetrical and Midwifery Model
Plus RED FLAGS to look for when hiring a provider
Is there a correct way to give birth? Is there a correct location with the least amount of risk? Is there a way to ensure that you will not only be alive on the other side but thrive? Pregnancy and birth are an intricate web of paths, decisions, and outcomes.
The truth is, there is no “one proper way” to give birth. Yes, God made women to be able to grow, give birth, and nourish their babies. But the path to get there will be as unique as each woman and baby. Therefore, the best you can do is gather as much information as you want and then make a decision that is best for your situation.
I believe this search should begin with prayer and discernment for where you see yourself on the spectrum of medicalization — more on that below. To have a peaceful and Christ-centered birth, you have to decide where you feel safe. Whether that’s at home with a midwife or in a group-practice medical suite, or somewhere in between, you can only know what’s best for you and your baby if you pray and research the different options.
Women-centered care that is respectful and compassionate is possible in every birth setting. But try not to settle on the most convenient; rather, create a team that truly sees you and your baby as the unique gift that you are, whether that’s in a hospital, birth center, home birth, or free birth.
*This information is for educational purposes only. No part of this article should be taken as medical advice.
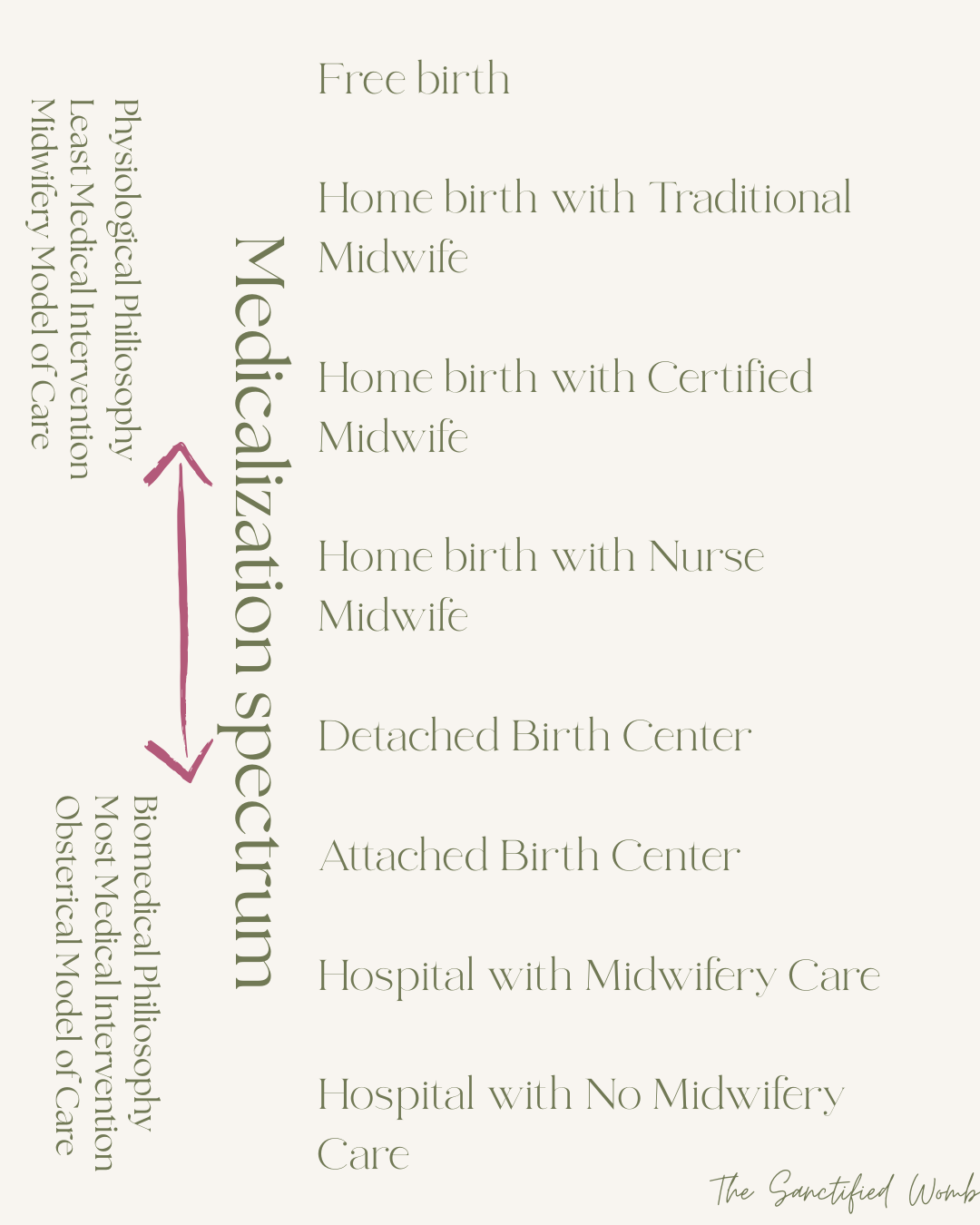
Spectrum of Medicalization
I first learned about this term from Dr. Melanie Jackson, a research and home-birth-based midwife in Australia. She discusses that on the spectrum of medicalization, you travel from the least intervention to the most intervention. And where each woman lands depends on her personal needs, wants, and specific pregnancy status.
On the chart, you’ll see that the least intervention occurs in a Free Birth with no medical attendant present, and the most intervention occurs in a private hospital with no midwifery influence. It is certainly possible to have a “mostly” physiological birth at a private hospital, but Jackson argues that leaving one’s home is the first intervention. Each mother must decide what is appropriate for her specific situation.
The Obstetrical Model of Care
As of 2020, 98% of women in the US give birth in the hospital and follow the same prenatal care regimen. Labor and birth are governed by the Obsterical model of care, where the doctors are highly skilled and trained to look for what could go wrong. Their expertise is in surgery and managing emergency situations.
Though there are some incredible providers out there, the system as a whole is set up as a conveyor belt to move as many women along as efficiently as possible, which means there is very little room for personalized care.
I’m not here to demonize the system or condemn it, but I do want to make it very clear that if you choose the system, you’re in their hands. For some women, that is safe and preferred. Hospitals and OBs are incredible. They save countless lives because of their emergency skills, but they put just as many (if not more) at risk because of their interventions. The trouble comes when they see every woman as a ticking time bomb, who could bleed out or explode if she chooses to go outside their “preferred” check list.
You must remember that God created women to grow, birth, and nourish their babies, and when we follow His design, it will work in the majority of situations. So, if you are set on a hospital birth, pray for your provider and your care team. Pray for the hospital and that your pregnancy and birth may be blessed and peaceful.
Conventional Prenatal Care
If you choose the obstetrical model, you’ll likely be in a group practice, meaning you’ll see a different provider every appointment and will get whatever doctor is “on-call” for the birth. You’ll follow a schedule of prenatal appointments where you're offered standardized “care and testing”.
In the United States, prenatal care generally looks like this:
You’ll be offered a dating ultrasound around 9-12 weeks.
First appointment for history and confirmation of pregnancy around 10-12 weeks. This appointment is usually with a Nurse Practitioner (NP).
Second trimester visits: once a month from 13 – 27 weeks, which assesses weight, blood pressure, doppler for baby’s heartbeat, fundal checks – asses the height of your growing uterus, and usually a 5-10 minute visit with the OB on call (or NP if no OB is available). They may also request a pap smear and blood work to check for baseline blood levels.
You may be offered numerous tests that check for different chromosomal issues and conditions.
You will be required to get a 20-week anatomy ultrasound to check on the baby’s growth and screen for potential growth abnormalities.
Around your 24-week check, you’ll be given a routine Gestational Diabetes test and potentially a Rhogam shot if you are Rh negative.
Third-trimester visits: twice a month from 28 – 35 weeks, once a week from 36 weeks to birth. You’ll be offered and often required to do a GBS (Group B Streptococcus) test around 35/36 weeks.
I can’t stress to you how important it is to research the benefits vs. risks for each test and procedure and prayerfully decide which, if any, are good for you. You do not have to do anything because of a policy. It’s your pregnancy and your baby. You are the one who has to live with the results of each intervention. For some mothers, every test offers peace of mind, and for others, it only creates anxiety and worry.
Pros. vs. Cons of the Obstetrical Model
As with any choice in life, there are many positive reasons to choose the obstetrical model of care. Countless women have exceptional experiences within the hospital birth setting. They feel seen and cared for. And there are likely just as many who did not have quite the same experience.
Pros of the Obstetrical Model
Prenatal care costs are usually covered by insurance
Doctors are expertly trained surgeons and are trained to see what may be wrong with labor and delivery
Access to pharmaceutical induction, pain relief, continuous fetal monitoring, or surgery
Access to the Neonatal Intensive Care Unit if your baby requires special care
Access to expert opinion for high-risk situations
Maybe good for a mother with anxiety to know she has all options at hand
Accessible to most women in the country
Cons of the Obstetrical Model
“One-size-fits-most” approach for prenatal care and labor setup
OBs get very little training in physiological birth or optimal nutrition
High induction and cesarean rate – over 30% for both
More likely to overestimate risk than to trust the birth process
Little to no continuity of care – you get whatever provider is on-call
Hospital’s are usually 17 years behind evidence-based practice
Once you start the “cascade of interventions,” it’s hard to stop
Limited mobility in labor and birth positions
Separation from the baby
Hospital policy adherence instead of mother-focused adherence
Limited access to doulas and midwives
Only one postpartum check at approximately 6 weeks
Use this list in your toolbox as you prayerfully create your birth team. Remember, there is no right or wrong place to give birth, just what brings you peace.
On the operating table after my induction turned into a cesarean section
The Midwifery Model of Care
On the flip side of the obstetrical care is the midwifery model of care.
In the US, we are not nearly as supportive of midwifery as other developed nations are. And we have a few different positions of midwives because the word “midwife” is not regulated in this country like it is in others, but there are different regulations on midwifery from state to state, which impact how they care for mothers. Some hospitals employ midwives, but more commonly, midwives practice at a birth center or home birth.
Nurse Midwives: A registered nurse who went to an accredited midwifery master’s program and tends to practice with a more medical mindset.
Certified Practicing Midwife: Goes through an accredited midwifery school and licensed with the state; can enter without prior healthcare experience.
Traditional Midwife: Followed a traditional apprenticeship with an experienced midwife to obtain education and birth observation experience.
Birth Keeper: Closely related to a traditional midwife but chooses not to take the traditional midwife title because they believe it has been tainted by modern midwifery practice.
Though there are differences between the different midwife titles, the care is similar and much more woman-focused. Philosophies of pregnancy and birth may differ from midwife to midwife, as she will be influenced by the schooling and personal philosophy she carries.
Ultimately, midwives are taught how physiological birth works and are experts in normal birth. They expect that a woman in their care is healthy and considered “low risk” in terms of health status. They support women to know their bodies and be a partner, if not a leader, in all decision-making.
Most of the prenatal care follows the obstetrical model of care, but there are a few very important differences.
Prenatal appointments are much more thorough, generally, 45-90 minutes long.
Appointments aren’t just about checking off the boxes of blood pressure, weight, and heartbeat checks. They try to build a relationship with the woman and her family.
They consider the mental, physical, spiritual, and emotional impact a pregnancy can have.
Midwives offer a thorough discussion of nutrition and how it impacts pregnancy, breastfeeding, and recovery.
There are usually alternative options for different prenatal tests and screenings, like the gestational diabetes test or the GBS test.
Overall, the midwifery model of care is much more woman-led and personalized. Midwives have the time to know each woman on a more personal level and understand what you want from your birth.
Moments after my successful vaginal birth after cesarean (VBAC)
Pros. vs. Cons of the Midwifery Model
It’s important to acknowledge that there are pros and cons to midwifery-led care as well. And just because your best friend or “that girl on Instagram” hired a midwife doesn’t mean you should blindly trust the only midwife you have access to. And remember, because midwives can practice in the hospital, home, and birth center, this list will vary depending on the location you choose.
Pros of the midwifery model of care
Midwives are experts in “low-risk” pregnancy care
Personalized care
Continuity of care – much more likely to have your midwife attend your birth, barring extraneous circumstances
Access to expert knowledge in physiological birth
More support for natural remedies
Support in nutrition and supplements
Often more comfortable and private (depending on birth location)
The mother is an active participant in birth choices and has a greater influence on the overall experience
Avoidance of unnecessary intervention
Usually lower cost (home vs. hospital)
Cultural and religious observations
More positive outcomes for vaginal birth and breastfeeding (most midwives have a less than 10% cesarean rate)
Cons of the midwifery model of care
Home birth midwives are not usually covered by insurance
Little to no access to pharmaceutical pain relief
Not trained in surgery
Not usually equipped to handle high-risk pregnancy and birth situations
If the need for a transfer arises, there may be a delay in care
Differing models of care between different midwives and locations
If a midwife is attached to hospital policy, they may be limited in their scope of practice
Lack of obstetrical support in needed cases
As you can see, choosing a provider, when in the obstetric model or midwifery model, should not be taken lightly. There are a lot of things to consider, and before you hire either, you should ask both your OB and Midwife many questions to make sure you’re on the same page.
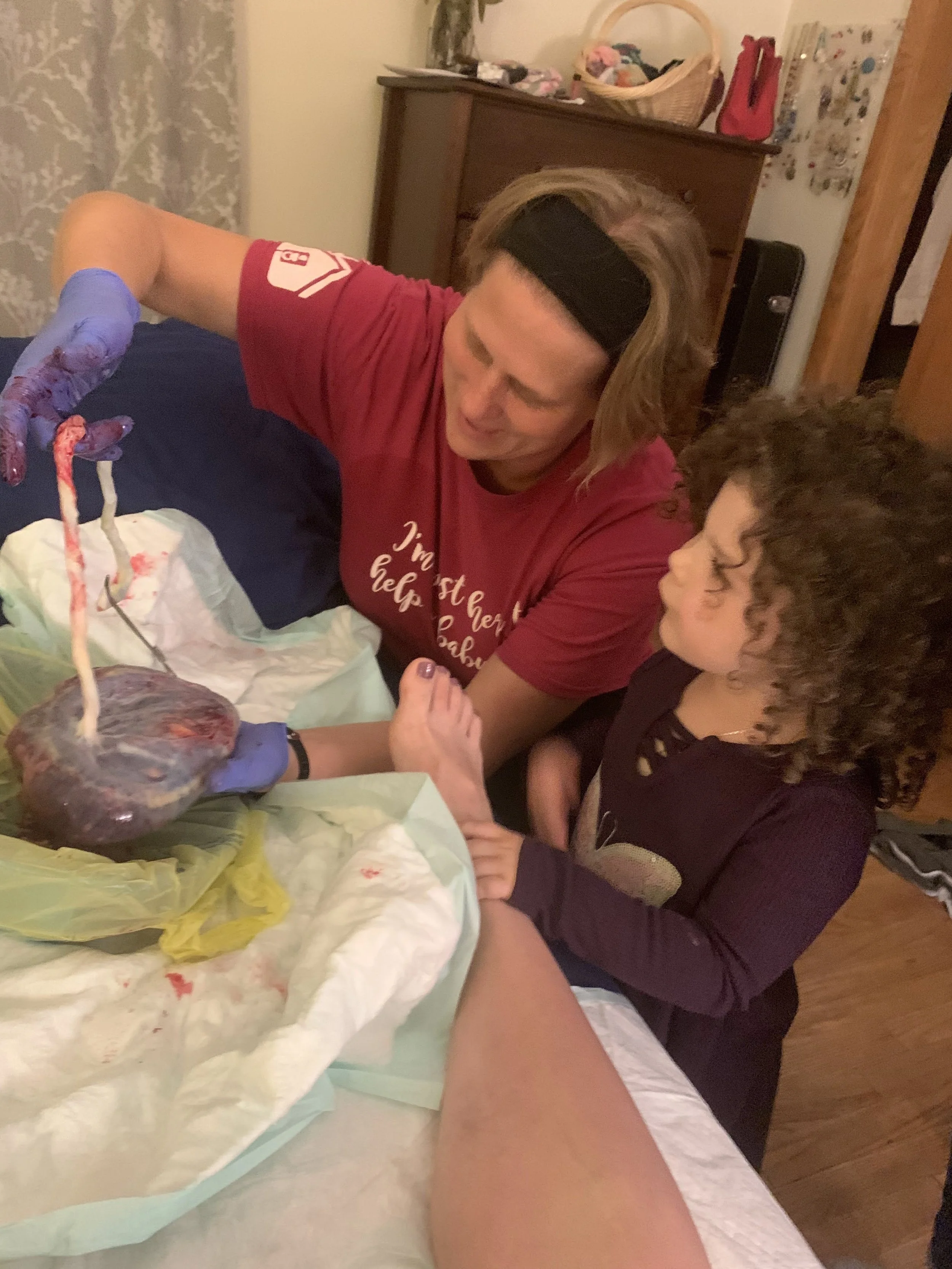
My incredible, Traditional midwife, showing my oldest her baby brothers placenta.
Find a provider who looks at your baby like this… whether that’s an OB or Midwife, you deserve to be 1 in a million.
Self-Led Prenatal Care
Outside of these two models of care is the growing movement of self-led prenatal care.
This model of care is growing in popularity with the free birth movement. Contrary to common propaganda, these women are usually more educated than the general population. They study physiological birth, often consult with experienced midwives, and spend a lot of time in prayer and reflection, preparing for birth.
The prenatal care is different from woman to woman as she focuses on what is best for her and her baby. They focus on nourishing foods, calm environments, connection to the womb, and God. Though many women in this space may be pagan, many Christian women are seeking to birth in this way with God alone as their guide.
Some use insurance to get blood work, ultrasounds, or seek “medical” advice. It’s safe to say that these women take their care very seriously and shouldn’t be considered reckless as a whole. Free birth comes with risk, just as birth in the hospital or home attended by a midwife does. Each woman should prayerfully and seriously consider what situation is best for them, taking into account their personal history and desired outcome.
RED Flags When Choosing a Provider
Whichever route you choose to go, you should be aware of a few RED flags. These usually give you an uneasy feeling in the pit of your stomach, make you want to cry or feel frustrated, or make you feel that something is just off. It can happen in the OB office or while sitting with a midwife, and I strongly encourage you to listen to your instincts.
These don’t always warrant firing your provider and seeking care somewhere else; rather, it’s an opportunity to tune in and figure out why you feel off and if what they’re saying really matters to you. This will be different for every woman and may change throughout the pregnancy and labor.
Situations or phrases to be aware of:
They don’t support natural or physiological birth
They see birth as a medical event that always needs intervention
They advise frequent ultrasounds with no clear reason why
They dismiss your birth plan/birth map
They don’t allow VBACs (vaginal birth after cesarean)
They don’t allow doula support
They say they “must” do an episiotomy with first-time moms
They start talking about inductions and scheduled cesarean sections early in care with no regard to medical need
They schedule an induction or cesarean section because your baby is “too big”
They schedule an induction because you’re past 41 weeks
A midwife says she cannot attend your birth after 42 weeks
A midwife or doctor says they must give you Pitocin after birth to prevent bleeding
A midwife says she will have an assistant midwife whom you will not meet before the birth
This list isn’t exhaustive, so be prayerful and aware and don’t ignore the voice in your head telling you to tune up.
Prenatal Care is Important – Don’t Make a Flippant Decision
Ultimately, whichever model of prenatal care you choose, be at peace. Find a team that supports you and encourages you. If you have a more medically complex pregnancy, find a provider who is an expert in your specific condition. And don’t be afraid to “shop around.” There is no need to hire the first OB or midwife you meet, and if something feels off, it’s *almost* never too late to find a different provider.